Overview
Bone cancer is a growth of cells that starts in a bone. Bone cancer can start in any bone. But it most often affects the thighbone.
The term "bone cancer" doesn't include cancer that starts in another part of the body and spreads to the bones. Instead, cancer that spreads to the bone is named for the place it began. For example, cancer that starts in the lungs and spreads to the bones is still lung cancer. Healthcare professionals might call it lung cancer that has metastasized to the bones.
Cancer that starts in the bones is rare. Different types of bone cancers exist. Some types of bone cancers mostly happen in children. Other types happen mostly in adults.
Common bone cancer treatments include surgery, radiation and chemotherapy. The best treatment for your bone cancer depends on the type of bone cancer, which bone is affected and other factors.
Symptoms
Signs and symptoms of bone cancer include:
- Bone pain.
- Swelling and tenderness near the affected area.
- Weakened bone, which can lead to a broken bone.
- Feeling very tired.
- Losing weight without trying.
When to see a doctor
Make an appointment with a doctor or other healthcare professional if you have any symptoms that worry you.
Causes
The cause of most bone cancers isn't known. Bone cancer starts when cells in or near a bone develop changes in their DNA. A cell's DNA holds the instructions that tell the cell what to do. In healthy cells, the DNA gives instructions to grow and multiply at a set rate. The instructions tell the cells to die at a set time. In cancer cells, the DNA changes give different instructions. The changes tell the cancer cells to make many more cells quickly. Cancer cells can keep living when healthy cells would die. This causes too many cells.
The cancer cells might form a mass called a tumor. The tumor can grow to invade and destroy healthy body tissue. In time, cancer cells can break away and spread to other parts of the body. When cancer spreads, it's called metastatic cancer.
Types of bone cancer
Bones contain a variety of different types of cells. Bone cancers are broken down into separate types, often based on the type of cell where the cancer began. The most common types of bone cancer include:
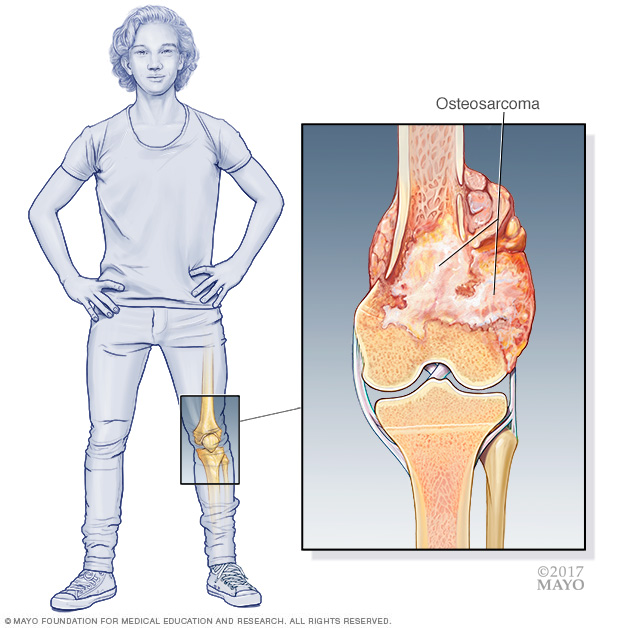
- Osteosarcoma. Osteosarcoma is a type of bone cancer that begins in the cells that form bones. It's the most common type of bone cancer. Osteosarcoma tends to happen most often in teenagers and young adults. But it also can happen in younger children and older adults. Osteosarcoma happens most often in the long bones of the legs and sometimes the arms. Very rarely, it happens in soft tissue outside the bone.
- Chondrosarcoma. Chondrosarcoma is a type of bone cancer that usually begins in the bones, but can sometimes occur in the soft tissue. Chondrosarcoma happens most often in the pelvis, hip and shoulder. It happens most often in middle-aged and older adults.
- Ewing sarcoma. Ewing sarcoma is a type of bone cancer that begins in the bones and the soft tissue around the bones. Ewing sarcoma mostly happens in children and young adults, although it can happen at any age. It most often begins in the leg bones and in the pelvis, but it can happen in any bone.
Risk factors
Things that increase the risk of bone cancer include:
- Inherited genetic syndromes. Certain rare genetic syndromes passed through families increase the risk of bone cancer. Examples include Li-Fraumeni syndrome and hereditary retinoblastoma.
- Other bone conditions. Some other bone conditions may increase the risk of bone cancer. The other bone conditions include Paget's disease of bone and fibrous dysplasia.
- Cancer treatment. Radiation therapy for cancer and some kinds of chemotherapy medicines used to treat cancer may increase the risk of bone cancer.
Healthcare professionals haven't found any ways to prevent bone cancer.
Diagnosis
Bone cancer diagnosis often involves imaging tests to look at the affected bone. To be certain whether a growth in the bones is cancer, a piece of tissue might be removed and tested for cancer cells.
Imaging tests
Imaging tests make pictures of the body. They can show the location and size of a bone cancer. Tests might include:
- X-ray.
- Magnetic resonance imaging, also called MRI.
- Computerized tomography scan, also called CT scan.
- Positron emission tomography scan, also called PET scan.
- Bone scan.
Biopsy
A biopsy is a procedure to remove a sample of tissue for testing in a lab. For bone cancer, the sample of tissue might be collected by:
- Inserting a needle through the skin. During a needle biopsy, a healthcare professional inserts a thin needle through the skin and guides it into the cancer. The health professional uses the needle to collect small samples of tissue.
- Removing the sample during surgery. During a surgical biopsy, a surgeon makes an incision in the skin to access the cancer. The surgeon removes a piece of the cancer for testing.
Determining the type of biopsy you need and the details of how to do the biopsy requires careful planning by your medical team. Healthcare professionals need to perform the biopsy in a way that won't interfere with future surgery to remove bone cancer. For this reason, ask for a referral to a healthcare team that treats a lot of bone cancers before your biopsy.
Stages of bone cancer
If you're found to have bone cancer, often the next step is to find out the extent of the cancer. This is called the cancer's stage. Your healthcare team uses your cancer's stage to help create your treatment plan. To determine the stage of the cancer, the healthcare team considers:
- The cancer's location.
- The size of the cancer.
- How fast the cancer is growing.
- The number of bones affected, such as number of affected vertebrae in the spine.
- Whether the cancer has spread to the lymph nodes or to other parts of the body.
The stages of bone cancer range from 1 to 4. A stage 1 bone cancer generally is a small cancer that is growing slowly. As the cancer grows larger or grows more quickly, the stages get higher. A stage 4 bone cancer has spread to the lymph nodes or to other parts of the body.
Treatment
Bone cancer treatments include surgery, radiation and chemotherapy. Which treatments are best for your bone cancer will depend on several factors. These factors include the type, location and stage of the bone cancer. Your healthcare team also considers your overall health and your preferences.
Surgery
The goal of surgery for bone cancer is to remove all of the cancer. The surgeon may remove the bone cancer and some of the healthy tissue around it. Then the surgeon repairs the bone. This might involve using a piece of bone from another part of your body. Sometimes the bone is repaired with metal or plastic material.
Sometimes surgeons need to remove an arm or leg in order to get all of the cancer, though this isn't common. It might be needed if the cancer grows very large or if the cancer is in a place that makes surgery difficult. After an arm or leg is removed, you may choose to use an artificial limb. With training and time with the new limb, you can learn to do everyday tasks.
Chemotherapy
Chemotherapy treats cancer with strong medicines. Many chemotherapy medicines exist. Most chemotherapy medicines are given through a vein. Some come in pill form.
Chemotherapy is often used after surgery for some types of bone cancers. It can kill any cancer cells that remain and lower the risk that the cancer will come back. Sometimes chemotherapy is given before surgery to shrink a bone cancer and make it easier to remove.
Not all types of bone cancers respond to chemotherapy treatments. Chemotherapy is often used to treat osteosarcoma and Ewing sarcoma. It's not often used for chondrosarcoma.
Radiation therapy
Radiation therapy treats cancer with powerful energy beams. The energy can come from X-rays, protons or other sources. During radiation therapy, you lie on a table while a machine moves around you. The machine directs radiation to precise points on your body.
Radiation therapy might be used after surgery to kill any bone cancer cells that might remain. It also might help control bone cancer when surgery isn't an option.
Some types of bone cancers are more likely to be helped by radiation therapy than others. Radiation therapy may be an option for treating Ewing sarcoma. It's not often used to treat chondrosarcoma or osteosarcoma.
Coping and support
A cancer diagnosis can feel overwhelming. With time you'll find ways to cope with the distress and uncertainty of cancer. Until then, you may find it helps to:
- Learn enough about bone cancer to make decisions about your care. Ask your healthcare team about your bone cancer, including your treatment options and, if you like, your prognosis. As you learn more about bone cancer, you may feel more confident in making treatment decisions.
- Keep friends and family close. Keeping your close relationships strong can help you deal with your bone cancer. Friends and family can provide the practical support you'll need, such as helping take care of your home if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by cancer.
- Find someone to talk with. Find a good listener who is willing to listen to you talk about your hopes and fears. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful. Ask your healthcare team about support groups in your area.
Preparing for an appointment
If you have any symptoms that worry you, start by making an appointment with a doctor or other healthcare professional. If your health professional suspects you may have bone cancer, you may be referred to a specialist. Bone cancer is often treated by a team of specialists that may include:
- Surgeons who operate on bones and joints, called orthopedic surgeons.
- Orthopedic surgeons who specialize in operating on cancers that affect the bones, called orthopedic oncologists.
- Doctors who specialize in treating cancer with medicine, called medical oncologists.
- Doctors who use radiation to treat cancer, called radiation oncologists.
- Doctors who analyze tissue to diagnose the specific type of cancer, called pathologists.
- Rehabilitation specialists who can help you recover after surgery.
How to prepare
Because appointments can be brief, it's a good idea to be prepared. Try to:
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you have, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements that you're taking.
- Consider taking a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who goes with you may remember something that you missed or forgot.
- Bring your previous scans or X-rays, the related reports and any other medical records important to this situation to the appointment.
Questions to ask
Preparing a list of questions can help you make the most of your time. List your questions from most important to least important in case time runs out. For bone cancer, some basic questions to ask include:
- What type of bone cancer do I have?
- What is the stage of my bone cancer?
- How quickly is my bone cancer growing?
- Will I need any additional tests?
- What are the treatment options for my bone cancer?
- What are the chances that treatment will cure my bone cancer?
- What are the side effects and risks of each treatment option?
- Will treatment make it impossible for me to have children?
- I have other health conditions. How will cancer treatments affect my other conditions?
- Is there one treatment that you think is best for me?
- What would you recommend to a friend or family member in my situation?
- Should I see a specialist? What will that cost, and will my insurance cover it?
- If I would like a second opinion, can you recommend a specialist?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
In addition to the questions that you've prepared, don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Be prepared to answer some questions about your symptoms and your health history. Questions may include:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
© 1998-2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


