Overview
Ataxia describes poor muscle control that causes clumsy movements. It can affect walking and balance, hand coordination, speech and swallowing, and eye movements.
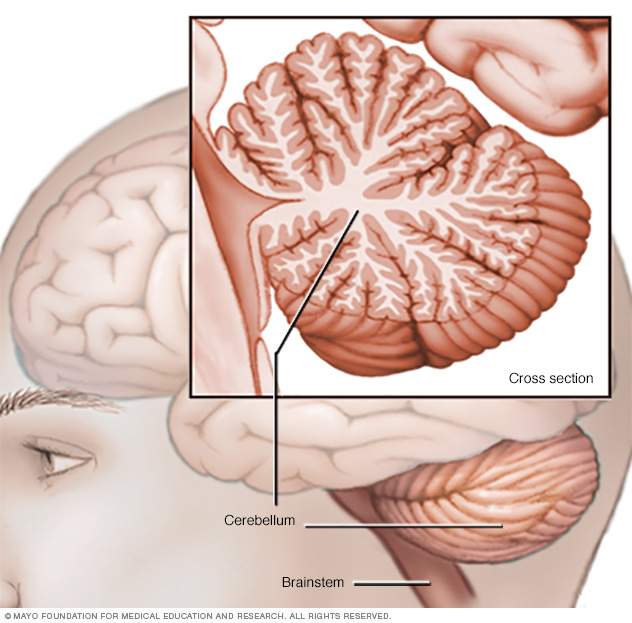
Ataxia usually results from damage to the part of the brain called the cerebellum or its connections. The cerebellum controls muscle coordination. Many conditions can cause ataxia, including genetic conditions, stroke, tumors, multiple sclerosis, degenerative diseases and alcohol misuse. Certain medicines also can cause ataxia.
Treatment for ataxia depends on the cause. Devices such as walkers and canes might help maintain independence. These also are called adaptive devices. Physical therapy, occupational therapy, speech therapy and regular exercise also might help.
Symptoms
Ataxia symptoms can develop over time or start suddenly. Ataxia can be a symptom of several nervous system conditions. Symptoms may include:
- Poor coordination.
- Walking unsteadily or with the feet set wide apart.
- Poor balance.
- Trouble with fine motor tasks such as eating, writing or buttoning a shirt.
- Changes in speech.
- Back-and-forth eye movements that can't be controlled.
- Trouble swallowing.
When to see a doctor
If you don't already have a condition that causes ataxia, such as multiple sclerosis, see your healthcare professional as soon as possible if you:
- Lose balance.
- Lose muscle coordination in a hand, arm or leg.
- Have trouble walking.
- Slur your speech.
- Have trouble swallowing.
Causes
Ataxia is caused by damage to the part of the brain called the cerebellum or its connections. The cerebellum is located at the base of the brain and connects to the brainstem. The cerebellum helps control balance, eye movements, swallowing and speech.
There are three major groups of ataxia causes: acquired, degenerative and hereditary.
Acquired causes
- Alcohol. Long-term excess alcohol use may cause persistent ataxia. Ataxia may improve by staying away from alcohol completely.
- Medicines. Ataxia is a potential side effect of certain medicines. It can be caused by sedatives such as phenobarbital and benzodiazepines. It also may be caused by anti-seizure medicines, especially phenytoin. Some types of chemotherapy also can cause ataxia.
- Toxins. Heavy metal poisoning, such as from lead or mercury, and solvent poisoning, such as from paint thinner, also can cause ataxia.
- Too little or too much of certain vitamins. Ataxia may be caused by not getting enough vitamin E, vitamin B-12 or vitamin B-1, also known as thiamine. Too little or too much vitamin B-6 also may cause ataxia. Not getting enough of a certain vitamin is known as a vitamin deficiency. When a vitamin deficiency is the cause of ataxia, it often can be reversed.
- Thyroid conditions. Hypothyroidism and hypoparathyroidism can cause ataxia.
- Stroke. Sudden onset of ataxia occurs with a stroke. This may be either due to a blood vessel blockage or bleeding on the brain.
- Multiple sclerosis. This condition may cause ataxia.
- Autoimmune diseases. Several diseases in which the immune system attacks healthy cells, known as autoimmune diseases, can cause ataxia. They can include a disease that causes inflammatory cells to collect in parts of the body, known as sarcoidosis. Or they may include an illness caused by an immune reaction to eating gluten, known as celiac disease. Ataxia also can be caused by certain types of a condition that results in swelling in the brain and spinal cord, called encephalomyelitis.
- Infections. Rarely, ataxia may be a symptom of chickenpox in childhood and other viral infections such as HIV and Lyme disease. It might appear in the healing stages of the infection and last for days or weeks. The symptom usually gets better over time.
- COVID-19. Ataxia can result from a serious infection with the virus that causes COVID-19.
- Paraneoplastic syndromes. These are rare degenerative conditions triggered by an immune system response to a cancerous tumor, known as a neoplasm. Paraneoplastic syndromes most often occur from lung, ovarian or breast cancer or lymphoma. Ataxia can appear months or years before the cancer is diagnosed.
- Changes in the brain. An infected area in the brain, known as an abscess, may cause ataxia. And a growth on the brain, such as a cancerous or noncancerous tumor, can damage the cerebellum.
- Head trauma. Brain damage may cause ataxia.
- Cerebral palsy. This is a general term for a group of conditions caused by damage to a child's brain. The damage may happen before, during or shortly after birth. It affects the child's ability to coordinate body movements.
Degenerative causes
- Multiple system atrophy. This rare condition affects movements and functions such as blood pressure. It can cause ataxia and other symptoms, including lack of bladder control, fainting after standing up and a sleep behavior condition in which a person acts out dreams.
Hereditary causes
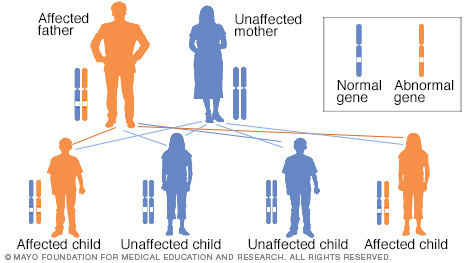
Some types of ataxia and some conditions that cause ataxia are passed down in families. These conditions also are called hereditary. If you have one of these conditions, you may have been born with a genetic change that causes the body to make irregular proteins.
The irregular proteins affect the function of nerve cells, primarily in the cerebellum and spinal cord. They cause the nerve cells to break down and die, known as degeneration. As the disease progresses, coordination problems worsen.
People with a genetic ataxia may have inherited a dominant gene from one parent, known as an autosomal dominant inheritance pattern. Or they may have inherited a recessive gene from both parents, known as an autosomal recessive inheritance pattern. In a recessive condition, the parents are not affected but siblings may be affected.
Different gene changes cause different types of ataxia. Most types get worse over time. Each type causes poor coordination but also has other specific symptoms.
Autosomal dominant ataxias
- Spinocerebellar ataxias. Researchers have identified more than 40 spinocerebellar ataxia genes, and the number continues to grow. Ataxia and cerebellar degeneration are common to all types, and there may be other symptoms.
-
Episodic ataxia (EA). There are eight recognized types of episodic ataxia. The types EA1 and EA2 are the most common. EA1 involves brief bouts of ataxia that may last seconds or minutes. The bouts are triggered by stress, sudden movement or being startled. They're often associated with muscle twitching.
EA2 involves longer bouts of ataxia, usually lasting from 30 minutes to six hours. These bouts also are triggered by stress. Dizziness and muscle weakness may occur. People with EA2 may feel very tired. Sometimes symptoms resolve later in life. Episodic ataxia doesn't shorten life span, and symptoms may respond to medicine.
Autosomal recessive ataxias
-
Friedreich ataxia. This is the most common hereditary ataxia. It involves damage to the cerebellum, spinal cord and peripheral nerves. Peripheral nerves carry signals from the arms and legs to the brain and spinal cord. Symptoms typically appear well before age 25. A brain scan usually doesn't show changes to the cerebellum with this type of ataxia.
The first symptom of Friedreich ataxia often is trouble walking. The condition typically goes on to affect the arms and trunk. This type of ataxia can cause changes to the feet, such as high arches. It also can cause a curve of the spine, known as scoliosis.
Other symptoms that might develop include slurred speech, fatigue, irregular eye movements and hearing loss. Friedreich ataxia also may lead to heart enlargement, known as cardiomyopathy. Heart failure and diabetes also can occur. Early treatment of heart conditions can improve quality of life and survival.
- RFC1-associated ataxia. This is the most common cause of ataxia that happens later in life. The ataxia symptoms usually occur with dizziness and numbness or tingling in the body. Sometimes this type of ataxia causes a cough.
-
Ataxia-telangiectasia. This rare childhood disease causes degeneration in the brain and immune system. This increases the risk of other diseases, including infections and tumors.
Telangiectasia is the formation of tiny red "spider" veins that might appear in the corners of a child's eyes or on the ears and cheeks. Delayed motor skill development, poor balance and slurred speech are often the first symptoms. Frequent sinus and respiratory infections are common.
Children with ataxia-telangiectasia are at high risk of developing cancer, particularly leukemia or lymphoma.
- Congenital cerebellar ataxia. This type of ataxia results from damage to the cerebellum that's present at birth.
- Wilson's disease. In people with this condition, copper builds up in the brain, liver and other organs. This can cause ataxia and other symptoms.
Risk factors
There are several risk factors for ataxia. People who have a family history of ataxia are at a higher risk of having ataxia themselves.
Other risk factors include:
- Drinking too much alcohol over a long period.
- Having hypothyroidism or hypoparathyroidism.
- Having multiple sclerosis.
- Having an illness caused by an immune reaction to eating gluten, known as celiac disease.
- Having a disease that causes inflammatory cells to build up in parts of the body, known as sarcoidosis.
- Having a degenerative disease called multiple system atrophy.
- Having a paraneoplastic syndrome triggered by cancer.
- Taking medicines that increase the risk of ataxia, such as anti-seizure medicines and sedatives.
- Being exposed to heavy metals, such as lead or mercury, or solvents, such as from paint thinner.
- Not getting enough vitamin E, vitamin B-6, vitamin B-12 or vitamin B-1, also known as thiamine. Getting too much vitamin B-6 also is a risk factor.
Diagnosis
When diagnosing ataxia, your healthcare professional looks for a treatable cause. You'll likely have physical and neurological exams. Your healthcare professional checks your vision, balance, coordination and reflexes. You also might need:
- Blood tests. These might help find treatable causes of ataxia.
- Imaging studies. An MRI of the brain might help find the possible causes. An MRI can sometimes show shrinkage of the cerebellum and other brain structures in people with ataxia. It also may show other treatable findings, such as a blood clot or benign tumor.
- A spinal tap, also known as lumbar puncture. This test may be helpful if an infection, swelling — also called inflammation — or certain diseases could be causing ataxia. A needle is inserted into the lower back between two bones to remove a small sample of cerebrospinal fluid. The fluid, which surrounds and protects the brain and spinal cord, is sent to a laboratory for testing.
- Genetic testing. Your healthcare professional might recommend genetic testing to see if a gene change may be causing a condition that leads to ataxia. Gene tests are available for many, but not all, hereditary ataxias.
Treatment
Ataxia treatment depends on the cause. If ataxia is caused by a condition such as vitamin deficiency or celiac disease, treating the condition may help improve symptoms. If ataxia results from chickenpox or other viral infections, it is likely to resolve on its own.
People with Friedreich ataxia can be treated with an oral medicine called omaveloxolone (Skyclarys). The U.S. Food and Drug Association approved the medicine for adults and teenagers 16 and older. In clinical trials, taking the medicine improved symptoms. People who take this medicine need regular blood tests because omaveloxolone can affect liver enzyme and cholesterol levels. Potential side effects of omaveloxolone include headache, nausea, stomach pain, fatigue, diarrhea, and muscle and joint pain.
Symptoms such as stiffness, tremor and dizziness might improve with other medicines. Your healthcare professional also might recommend adaptive devices or therapies.
Adaptive devices
Ataxia caused by conditions such as multiple sclerosis or cerebral palsy might not be treatable. But adaptive devices may help. They include:
- Hiking sticks or walkers for walking.
- Modified utensils for eating.
- Communication aids for speaking.
Therapies
You might benefit from certain therapies, including:
- Physical therapy to help with coordination and enhance mobility.
- Occupational therapy to help with daily living tasks, such as feeding yourself.
- Speech therapy to improve speech and aid swallowing.
Some studies have found that aerobic and strength exercises may be beneficial for some people with ataxia.
Coping and support
Living with ataxia or having a child with the condition can be challenging. For some people, having ataxia may lead to depression and anxiety. Talking with a counselor or therapist might help. Joining a support group for ataxia or for a condition causing ataxia may provide information and encouragement.
Support group members often know about the latest treatments and tend to share their own experiences. Your healthcare professional might be able to recommend a group in your area.
Preparing for an appointment
You're likely to start by seeing your healthcare professional. You may be referred to a neurologist.
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before having a specific test.
Make a list of:
- Your symptoms, including any that may seem unrelated to the reason for which you scheduled the appointment, and when they began.
- Key personal information, including other conditions you have and family medical history.
- All medicines, vitamins or supplements you take, including doses.
- Questions to ask your healthcare professional.
Take a family member or friend along, if possible, to help you remember the information you get.
For ataxia, basic questions to ask include:
- What is likely causing my symptoms?
- Other than the most likely cause, what are other possible causes?
- What tests do I need?
- Is my condition likely temporary or chronic?
- What's the best course of action?
- Are there devices that can help me with coordination?
- I have other health conditions. How can I best manage them together?
- Are there restrictions I need to follow?
- Should I see a specialist?
- Are there brochures or other printed material I can take with me? What websites do you recommend?
- Do you know of ataxia research studies I might participate in?
Don't hesitate to ask other questions.
What to expect from your doctor
Your healthcare professional is likely to ask you questions, such as:
- When did your symptoms start?
- What was your first symptom?
- Do you notice your symptoms all the time, or every once in a while?
- What seems to improve your symptoms?
- What seems to worsen your symptoms?
- Do you have family members who have had these types of symptoms?
- Do you use alcohol or drugs?
- Have you been exposed to toxins?
- Have you had an infection with a virus recently?
What you can do in the meantime
Don't drink alcohol or take legal or illegal drugs that may be sold on the street, also called recreational drugs, which can make your ataxia worse.
© 1998-2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


