Overview
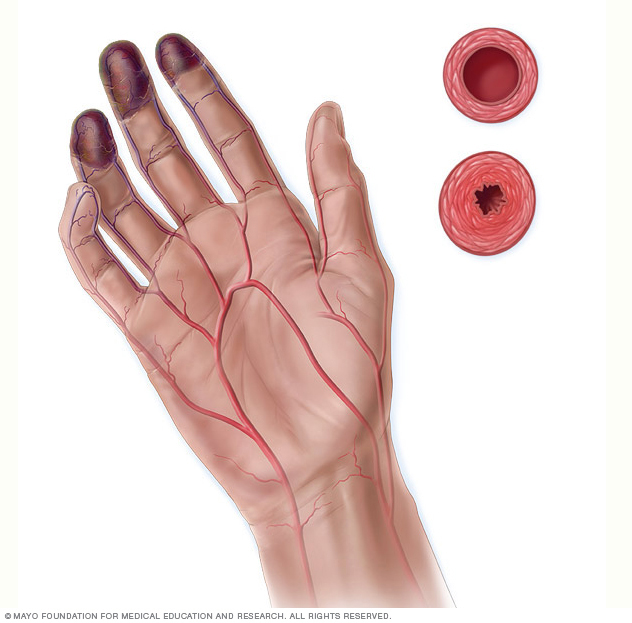
Buerger disease is a rare disease of the arteries and veins in the arms and legs. In Buerger disease — also called thromboangiitis obliterans — blood vessels become blocked. This reduces blood flow to the affected areas. Blood clots may form in the blood vessels.
Over time, the lack of blood flow damages or destroys skin tissue. The damage can lead to infection and death of body tissue, called gangrene. Buerger disease is usually first seen in the feet. It may eventually affect the blood vessels of the hand. Blood clots may form in the small veins of the arms and legs.
People who get Buerger disease almost always smoke cigarettes or use other forms of tobacco, such as chewing tobacco. Quitting all forms of tobacco is the only way to stop Buerger disease. For those who don't quit, surgery to remove fingers and toes might be needed.
Symptoms
Buerger disease symptoms include:
- Tingling or numbness in the fingers or toes.
- Changes in skin color in the hands and feet. The skin may look pale gray, red or blue. Depending on your skin color, these color changes may be harder or easier to see.
- Fingers and toes that turn white then blue when exposed to cold, known as Raynaud's disease. Depending on your skin color, these color changes may be harder or easier to see.
- Pain in the feet that occurs with walking. The pain may make it difficult to walk long distances.
- Painful open sores on fingers and toes. Pain in the fingers and toes may become severe and occur at rest.
- Inflammation of a vein just below the skin's surface, due to a blood clot in the vein.
When to see a doctor
See a health care provider if you think you have symptoms of Buerger disease.
Causes
The exact cause of Buerger disease is unknown. The condition is strongly linked to tobacco use. It's thought that chemicals in tobacco may hurt the lining of the blood vessels.
Experts think that some people have genes that make them more likely to get Buerger disease. It's also possible that the disease occurs when the body's immune system attacks healthy tissue by mistake.
Risk factors
The biggest risk factor for Buerger disease is smoking or using any type of tobacco. The disease can occur in people who smoke cigarettes, use cigars and chew tobacco. The rates of Buerger disease are highest in areas of the Mediterranean, Middle East and Asia where heavy smoking is most common.
Some research says that long-term use of marijuana, also called cannabis, also raises the risk of blood vessel problems similar to those of Buerger disease.
Other risk factors for Buerger disease include being male and being younger than 45 years old. Long-term infection of the gums in the mouth may also increase the risk. But more study is needed to confirm this link.
Complications
Buerger disease decreases blood flow to the hands and feet. As the disease gets worse, the skin and tissue in the affected areas do not get enough blood. This can cause painful open sores that do not heal. The sores may lead to a complication called gangrene.
Symptoms of gangrene include black or blue skin, a loss of feeling in the affected finger or toe, and a bad smell from the area. Gangrene is a serious condition. Surgery is usually needed to remove the affected finger, toe or other tissue.
Prevention
Nearly everyone who has Buerger disease has smoked or used some form of tobacco. To prevent Buerger disease, it's important to not use tobacco.
Quitting smoking can be hard. Talk to a health care provider about ways to quit.
Diagnosis
There's no test that can diagnose Buerger disease. But tests can be done to check for other common conditions that may cause similar symptoms.
Tests may include:
- Blood tests. Blood tests may be done to check for diabetes, blood-clotting disorders, or autoimmune diseases such as scleroderma or lupus.
- Exam of the arteries in hands and feet. Blood pressure cuffs and ultrasound imaging are used to see how blood moves through the hands and feet. This test is often done in a special vascular laboratory. But it can be done at a medical provider's office. Other tests may be done to check blood flow to the skin.
- CT or MRI scan of the blood vessels. These tests show blood flow in the arteries. Before the images are taken, a special dye may be given by IV. The dye helps the arteries show up more clearly on the images.
- Angiogram of the hands and feet. This invasive test helps health care providers see blockages in the very small blood vessels of the hands and feet. A long, thin flexible tube called a catheter is inserted into a blood vessel. Dye, also called contrast, flows through the catheter to arteries in the heart. The dye helps the arteries show up more clearly on X-ray images and video.
Treatment
There's no cure for Buerger disease. The only proven treatment for Buerger disease is to quit using all tobacco products. Even one cigarette a day can make the disease worse. This includes using electronic cigarettes, vaping and using marijuana.
If you have Buerger disease and smoke or use tobacco in any form, talk to your health care provider about ways to quit. Nicotine replacement products aren't an option because they still have nicotine in them. Nicotine is thought to irritate the blood vessels. Your health care provider can recommend other medicines that might help.
Another option is a live-in program to help you stop smoking. You typically stay at a treatment center or hospital for a few days or weeks. You'll learn how to stop cravings for cigarettes and how to live tobacco-free.
Other treatments for Buerger disease symptoms are available, but they don't work as well as quitting smoking. Those treatments may include medicines, compression therapy and surgery.
Medicines
If you have Buerger disease, your health care provider may recommend medicine to improve blood flow. For example, some blood pressure medicines may be helpful. Aspirin may be given to prevent blood clots.
A medicine called bosentan (Tracleer) may be tried if you have very severe Buerger disease symptoms. It's approved to treat high blood pressure in the lungs. But a few studies showed that it improved blood flow in people with Buerger disease.
Other medicines depend on your symptoms and other health conditions. Medicines may be given to treat pain or heal skin sores.
Therapies
If you have Buerger disease, your provider may suggest a medicine-free treatment called compression therapy. Your health care provider may call this treatment intermittent pneumatic compression pumping. This treatment puts pressure on the affected body area to improve blood flow.
During compression therapy, you wear a sleeve over the affected arm or leg. The sleeve connects to a pump. The pump sends air into the sleeve on and off. The sleeve inflates, gently squeezing the affected body area. The pressure increases blood flow to the area.
Surgery or other procedures
Buerger disease causes a severe lack of blood flow, which can damage skin tissue or cause it to die. Surgery may be needed to remove an arm or leg that's infected or has dead tissue. This surgery is called amputation.
Lifestyle and home remedies
To improve symptoms of Buerger disease and prevent complications, take the following steps:
- Exercise. Regular exercise helps improve blood flow. With your provider's OK, aim for 30 to 60 minutes of physical activity most days of the week. Talk to your health care provider about the amount and type of exercise that's best for you.
- Check your skin. Buerger disease can cause a loss of feeling in the fingers, toes and other body areas. So an injury to the skin might go unnoticed. Check every day for cuts and scrapes on the arms and legs. Protect fingers and toes from cold and injury.
- Clean cuts and scrapes. A lack of blood flow to the arms and legs increases the risk of infection. Even small cuts and scrapes can turn into serious infections. Always clean cuts and scrapes with soap and water to prevent infection. Apply antibiotic ointment and cover the cuts with clean bandages. If a skin injury gets worse or heals slowly, see a health care provider quickly.
- Take care of your teeth and gums. Visit a dentist regularly to keep gums and teeth in good health. Long-term gum disease is linked to Buerger disease.
- Do not smoke tobacco, vape or use marijuana. Not smoking is the best way to prevent and manage Buerger disease. Also avoid vaping, e-cigarettes and marijuana. It's also important to stay away from smoke from all burning tobacco products and the smoke a tobacco user breathes out. This type of smoke is called secondhand smoke. Any amount of secondhand smoke is bad for the heart and blood vessels.
Preparing for an appointment
You're likely to start by seeing your primary care provider. If you have symptoms of Buerger disease, you may be referred to a provider trained in blood vessel diseases. This type of health care provider is called a vascular specialist.
What you can do
Take someone along to your health care provider's visit, if possible. Someone who goes with you can help you remember information you're given.
Make a list of:
- Your symptoms, including any that may not seem to be related to Buerger disease. Note when the symptoms began.
- Important personal information, such as if you've ever smoked or used any tobacco products. Also note if you've ever worked with vibrating tools such as a jackhammer, which can cause blood vessel injuries to the hands or feet.
- All medicines, vitamins or supplements you take. Include the doses.
- Questions to ask your health care provider.
Some basic questions to ask include:
- What's the most likely cause of my symptoms?
- What tests do I need?
- What are the treatment options? Which do you recommend?
- I have other health conditions. How can I best manage these conditions together?
- Should I see a specialist?
- Are there brochures or other printed materials that I can have? What websites do you recommend?
Don't hesitate to ask other questions as well.
What to expect from your doctor
Your health care provider might ask:
- Do you have symptoms all the time, or do they come and go?
- How bad are your symptoms?
- Does anything seem to make your symptoms better?
- What, if anything, makes your symptoms worse?
- Do your fingers change color in the cold?
© 1998-2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


