Overview
De Quervain tenosynovitis (dih-kwer-VAIN ten-oh-sine-oh-VIE-tis) is a painful condition affecting the tendons on the thumb side of the wrist. If you have de Quervain tenosynovitis, you will probably feel pain when you turn your wrist, grasp anything or make a fist.
Although the exact cause of de Quervain tenosynovitis isn't known, any activity that relies on repetitive hand or wrist movement — such as working in the garden, playing golf or racket sports, or lifting a baby — can make it worse.
Symptoms
Symptoms of de Quervain tenosynovitis include:
- Pain near the base of the thumb
- Swelling near the base of the thumb
- Difficulty moving the thumb and wrist when doing something that involves grasping or pinching
- A "sticking" or "stop-and-go" sensation in the thumb when moving it
If the condition goes too long without treatment, the pain may spread farther into the thumb or forearm or both. Moving the thumb and wrist may make the pain worse.
When to see a doctor
Consult your health care provider if you're still having problems with pain or function and you've already tried:
- Not using your affected thumb
- Applying cold to the affected area
- Using nonsteroidal anti-inflammatory drugs, such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve)
Causes
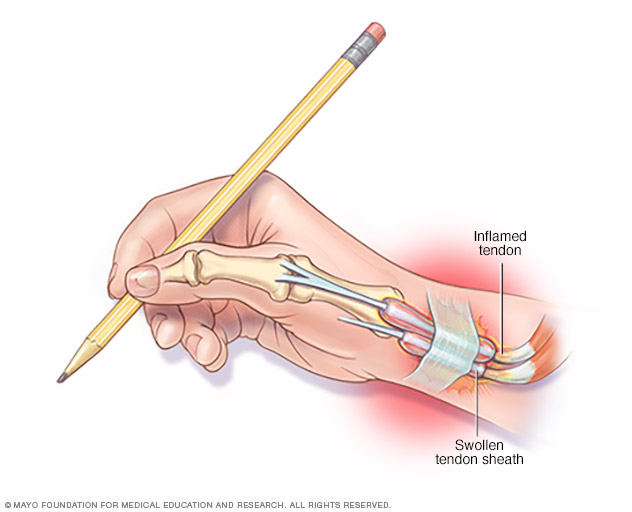
De Quervain tenosynovitis affects the two tendons on the thumb side of the wrist. Tendons are ropelike structures that attach muscle to bone.
Chronic overuse, such as repeating a particular hand motion day after day, may irritate the covering around the tendons. If the covering becomes irritated, the tendons can thicken and swell. This thickening and swelling restrict the movement of the tendons through the small tunnel that connects them to the base of the thumb.
Other causes of de Quervain tenosynovitis include:
- Inflammatory arthritis, such as rheumatoid arthritis.
- Direct injury to the wrist or tendon, which may cause scar tissue that restricts movement of the tendons
- Fluid retention, such as from changes in hormones during pregnancy
Risk factors
Risk factors for de Quervain tenosynovitis include:
- Age. People between the ages of 30 and 50 have a higher risk of developing de Quervain tenosynovitis than do people in other age groups, including children.
- Sex. The condition is more common in women.
- Being pregnant. The condition may be associated with pregnancy.
- Baby care. Lifting a child repeatedly involves using the thumbs as leverage and may be associated with the condition.
- Jobs or hobbies that involve repetitive hand and wrist motions. These may contribute to de Quervain tenosynovitis.
Complications
When de Quervain tenosynovitis goes untreated, it can become difficult to use the hand and wrist properly. The wrist may lose some range of motion.
Diagnosis
To diagnose de Quervain tenosynovitis, your health care provider will examine your hand to see if you feel pain when pressure is applied on the thumb side of the wrist.
Tests
You may be asked to perform a Finkelstein test, in which you bend your thumb across the palm of your hand and bend your fingers down over your thumb. Then you bend your wrist toward your little finger. If this causes pain on the thumb side of your wrist, you likely have de Quervain tenosynovitis.
Imaging tests, such as X-rays, generally aren't needed to diagnose de Quervain tenosynovitis.
Treatment
Treatment for de Quervain tenosynovitis is aimed at reducing inflammation, preserving movement in the thumb and preventing recurrence.
If you start treatment early, your symptoms should improve within 4 to 6 weeks. If de Quervain tenosynovitis starts during pregnancy, symptoms are likely to end around the end of either pregnancy or breastfeeding.
Medications
To reduce pain and swelling, your doctor may recommend using pain relievers that you can buy without a prescription. These include ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve).
Your doctor may also recommend injections of corticosteroid medications into the tendon covering to reduce swelling. If treatment begins within the first six months of symptoms, most people recover completely after receiving corticosteroid injections, often after just one injection.
Therapies
Initial treatment of de Quervain tenosynovitis may include:
- Immobilizing the thumb and wrist, keeping them straight with a splint or brace to help rest the tendons
- Avoiding repetitive thumb movements as much as possible
- Avoiding pinching with the thumb when moving the wrist from side to side
- Applying ice to the affected area
You may also see a physical therapist or an occupational therapist. The therapist may review how you use your wrist and give suggestions on how to relieve stress on your wrists. Your therapist can also teach you exercises for your wrist, hand and arm. These exercises can strengthen your muscles, reduce pain and limit tendon irritation.
Surgery or other procedures
Surgery may be recommended for more-serious cases. The surgery is outpatient. In the procedure, the surgeon inspects the sheath surrounding the involved tendon or tendons and then opens the sheath to release the pressure. This allows the tendons to glide freely.
Your health care provider will talk to you about how to rest, strengthen and rehabilitate your body after surgery. A physical therapist or an occupational therapist may meet with you after surgery to teach you new strengthening exercises and help you adjust your daily routine to prevent future problems.
Lifestyle and home remedies
If you don't need surgery, caring for your condition is much the same as preventing it:
- Avoid moving your wrists the same way repeatedly.
- Wear a brace or splint if suggested by your health care provider.
- Follow through with recommended exercises.
- Note activity that causes pain, swelling or numbness in your thumb and wrist. Try to avoid this activity and share the information with your provider.
Preparing for an appointment
Make an appointment with your health care provider if you have hand or wrist pain and if avoiding the activities that trigger the pain aren't helping. After an initial exam, you may be referred to an orthopedist, a rheumatologist, a hand therapist or an occupational therapist.
Here's some information to help you get ready for your appointment.
What you can do
- Write down key medical information, including other conditions you have and all medications and supplements you're taking.
- Note hobbies and activities that may strain your hand or wrist, such as knitting, gardening, playing an instrument, participating in racket sports or performing repetitive workplace activities.
- Note any recent injuries to your hand or wrist.
- Write down questions to ask your doctor.
Below are some basic questions to ask the health care provider who evaluates you for wrist- or hand-related symptoms.
- What is the most likely cause of my symptoms?
- Are there other possible causes?
- Do I need tests to confirm the diagnosis?
- What treatment do you recommend?
- I have other health problems. How can I best manage these conditions together?
- Will I need surgery?
- How long will I need to avoid the activities that caused my condition?
- What else can I do on my own to improve my condition?
Don't hesitate to ask other questions as well.
What to expect from your doctor
A health care provider who sees you for symptoms common to de Quervain tenosynovitis may ask a number of questions. You might be asked:
- What are your symptoms and when did they begin?
- Have your symptoms been getting worse or staying the same?
- What activities seem to trigger your symptoms?
- Do you participate in any hobbies or sports that involve repetitive hand or wrist movements?
- What tasks do you perform at work?
- Have you recently had an injury that may have damaged your hand or wrist?
- Does it help to avoid the activities that trigger your symptoms?
- Have you tried at-home treatments, such as nonprescription pain relievers? What, if anything, helps?
© 1998-2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


