Overview
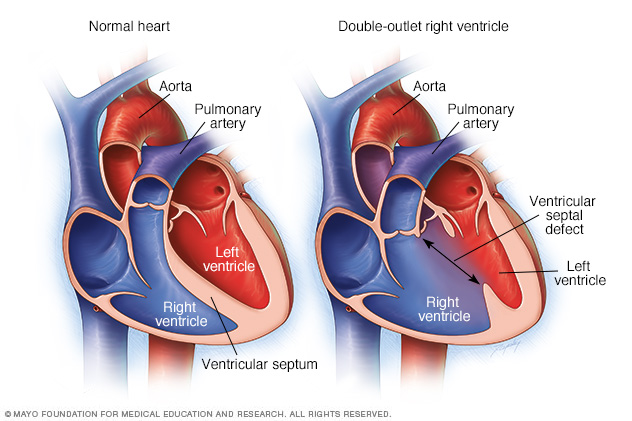
Double-outlet right ventricle is a heart condition present at birth. That means it's a congenital heart defect. In this condition, the body's main artery and the lung artery do not connect to the usual areas in the heart. The body's main artery is called the aorta. The lung artery is called the pulmonary artery.
Sometimes these blood vessels also are reversed from their usual positions.
In a typical heart, the aorta connects to the left lower heart chamber. The pulmonary artery connects to the right lower heart chamber.
In babies with double-outlet right ventricle, both the aorta and the pulmonary artery connect partially or completely to the right lower heart chamber.
Babies with double-outlet right ventricle also have a hole between the lower heart chambers. The lower heart chambers are called the ventricles. The hole is called a ventricular septal defect. The hole causes oxygen-rich blood to mix with oxygen-poor blood. Babies with this condition may not get enough oxygen in the bloodstream. Their skin may appear gray or blue.
Double-outlet right ventricle may occur with other heart problems present at birth. These problems may include other holes in the heart, heart valve problems or blood vessel problems.
Complications
If too much blood flows through the pulmonary artery to the lungs, it can lead to heart failure and poor growth.
Diagnosis
A test called an echocardiogram can diagnose double-outlet right ventricle. The test uses sound waves to create images of the beating heart. It can show blood flow through the heart and heart valves.
If more details about the heart are needed, other tests may be done. Tests to check the heart may include:
- Heart CT scan. Also called a cardiac CT, this test uses X-rays to create cross-sectional images of specific parts of the body.
- Heart MRI scan. This test uses magnetic fields and radio waves to create detailed images of the heart.
- Cardiac catheterization. The provider inserts a long, thin flexible tube called a catheter into a blood vessel, usually in the groin or wrist. It's guided to the heart. Dye flows through the catheter to arteries in the heart. The dye helps the arteries show up more clearly on X-ray images and video. During this test, the provider can measure pressure and oxygen levels in the chambers of the heart and in the blood vessels.
Treatment
Some babies with double-outlet right ventricle need heart repair surgery within the first few days of birth. Others may have surgery at a few months of age.
More than one type of surgery may be done. The type of surgery depends on the specific heart problems.
The heart surgeon may do one or more of the following:
- Create a tunnel through the hole in the heart to connect the left ventricle to the aorta.
- Correct the aorta and pulmonary artery positions, if they're reversed.
- Patch the hole between the lower heart chambers.
- Insert a blood vessel to connect the right ventricle to the pulmonary artery. This lets more blood flow if the pulmonary artery is small.
- Widen a narrowed pulmonary artery to allow more blood flow.
- Repair any other heart problems present at birth.
In some newborn babies, a temporary procedure using a tube called a shunt may be done to increase blood flow to the lungs. The heart surgeon places the shunt between the baby's aorta and the pulmonary artery. The shunt is removed later in life during heart surgery to repair the double-outlet right ventricle.
A person born with double-outlet right ventricle needs regular health checkups for life. Adults should see a health care provider trained in evaluating and treating congenital heart conditions. This type of provider is called an adult congenital cardiologist.
Later in life, surgery may be needed if a heart valve is narrowed or leaks blood backward.
Some adults born with double-outlet right ventricle need medicine to help the right or left lower heart chambers work better.
© 1998-2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


