Overview
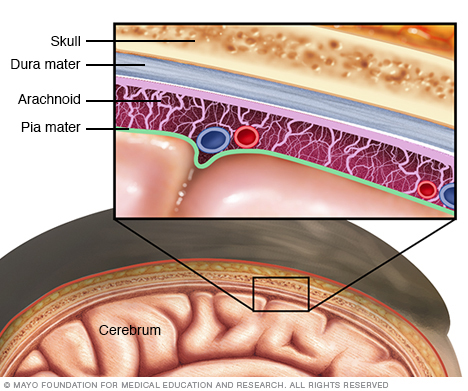
Meningitis is an infection and inflammation of the fluid and membranes surrounding the brain and spinal cord. These membranes are called meninges.
The inflammation from meningitis typically triggers symptoms such as headache, fever and a stiff neck.
Most cases of meningitis in the United States are caused by a viral infection. But bacteria, parasites and fungi also can cause it. Some cases of meningitis improve without treatment in a few weeks. Others can cause death and require emergency antibiotic treatment.
Seek immediate medical care if you suspect that you or someone in your family has meningitis. Early treatment of bacterial meningitis can prevent serious complications.
Symptoms
Early meningitis symptoms may be similar to the flu. Symptoms may develop over several hours or over a few days.
Possible symptoms in anyone older than the age of 2 years include:
- Sudden high fever.
- Stiff neck.
- Severe headache.
- Nausea or vomiting.
- Confusion or trouble concentrating.
- Seizures.
- Sleepiness or trouble waking.
- Sensitivity to light.
- No appetite or thirst.
- Skin rash in some cases, such as in meningococcal meningitis.
Signs in newborns
Newborns and infants may show these signs:
- High fever.
- Constant crying.
- Being very sleepy or irritable.
- Trouble waking from sleep.
- Being inactive or sluggish.
- Not waking to eat.
- Poor feeding.
- Vomiting.
- A bulge in the soft spot on top of the baby's head.
- Stiffness in the body and neck.
Infants with meningitis may be hard to comfort. They may even cry harder when held.
When to see a doctor
Seek immediate medical care if you or someone in your family has meningitis symptoms, such as:
- Fever.
- Severe headache that doesn't go away.
- Confusion.
- Vomiting.
- Stiff neck.
Bacterial meningitis is serious and can cause death within days without prompt antibiotic treatment. Delayed treatment also increases the risk of permanent brain damage.
It's also important to talk to your health care provider if you've been exposed to someone with meningitis. That may include a family member or someone you live or work with. You may need to take medicines to prevent getting an infection.
Causes
Viral infections are the most common cause of meningitis. That's followed by bacterial infections and, rarely, fungal and parasitic infections. Because bacterial infections can lead to death, learning the cause is essential.
Bacterial meningitis
Bacteria that enter the bloodstream and travel to the brain and spinal cord cause bacterial meningitis. But bacterial meningitis also can occur when bacteria directly invade the meninges. This may be caused by an ear or sinus infection, a skull fracture, or — rarely — some surgeries.
Several strains of bacteria can cause bacterial meningitis, most commonly:
- Streptococcus pneumoniae. This bacterium is the most common cause of bacterial meningitis in infants, young children and adults in the United States. It more commonly causes pneumonia or ear or sinus infections. A vaccine can help prevent this infection.
-
Neisseria meningitidis. This bacterium causes a bacterial meningitis called meningococcal meningitis. These bacteria commonly cause an upper respiratory infection but can cause meningococcal meningitis when they enter the bloodstream. This is a highly contagious infection that affects mainly teenagers and young adults. It may cause local epidemics in college dormitories, boarding schools and military bases.
A vaccine can help prevent infection. Even if vaccinated, anybody who has been in close contact with a person with meningococcal meningitis should receive an oral antibiotic to prevent the disease.
- Haemophilus influenzae. Haemophilus influenzae type b (Hib) bacterium was once the leading cause of bacterial meningitis in children. But new Hib vaccines have greatly reduced the number of cases of this type of meningitis.
- Listeria monocytogenes. These bacteria can be found in unpasteurized cheeses, hot dogs and lunchmeats. People who are pregnant, newborns, older adults and people with weakened immune systems are most susceptible. During pregnancy, listeria can cross the placenta. Infections in late pregnancy may be fatal to the baby.
Viral meningitis
Viral meningitis is usually mild and often clears on its own. Most cases in the United States are caused by a group of viruses known as enteroviruses. They're most common in late summer and early fall. Viruses such as herpes simplex virus, HIV, mumps virus, West Nile virus and others also can cause viral meningitis.
Chronic meningitis
Chronic meningitis — one that's long-lasting — can be caused by slow-growing organisms such as fungi and Mycobacterium tuberculosis. They invade the membranes and fluid surrounding the brain. Chronic meningitis develops over two weeks or more. Symptoms are similar to acute meningitis, which is a sudden, new case. They include headache, fever, vomiting and mental cloudiness.
Fungal meningitis
Fungal meningitis isn't common in the United States. It may mimic acute bacterial meningitis. It's often contracted by breathing in fungal spores that may be found in soil, decaying wood and bird droppings.
Fungal meningitis isn't spread from person to person. Cryptococcal meningitis is a common fungal form of the disease. It affects people with weakened immune systems, such as from AIDS. It can cause death if not treated with an antifungal medicine. Even with treatment, fungal meningitis may come back.
Parasitic meningitis
Parasites can cause a rare type of meningitis called eosinophilic meningitis. Parasitic meningitis also can be caused by a tapeworm infection in the brain or cerebral malaria. Amoebic meningitis is a rare type that is sometimes contracted through swimming in fresh water and can quickly become life-threatening.
The main parasites that cause meningitis typically infect animals. People are usually infected by eating foods contaminated with these parasites. Parasitic meningitis isn't spread between people.
Other meningitis causes
Meningitis also can result from noninfectious causes. They include chemical reactions, drug allergies, some types of cancer and inflammatory diseases such as sarcoidosis.
Risk factors
Risk factors for meningitis include:
- Skipping vaccinations. Risk rises for anyone who hasn't completed the recommended childhood or adult vaccination schedule.
- Age. Most cases of viral meningitis occur in children younger than age 5 years. Bacterial meningitis is common in those under age 20.
- Living in a community setting. College students living in dormitories, personnel on military bases, and children in boarding schools and child care facilities are at greater risk of meningococcal meningitis. This is probably because the bacterium is spread through the respiratory route, and spreads quickly through large groups.
- Pregnancy. Pregnancy increases the risk of an infection caused by listeria bacteria, which also may cause meningitis. The infection increases the risk of miscarriage, stillbirth and premature delivery.
- Weakened immune system. AIDS, alcohol use disorder, diabetes, use of immunosuppressant drugs and other factors that affect your immune system increase the risk of meningitis. Having a spleen removed also increases risk. People without a spleen should get vaccinated to lower the risk.
Complications
Meningitis complications can be severe. The longer you or your child has the disease without treatment, the greater the risk of seizures and permanent neurological damage, including:
- Hearing loss.
- Memory problems.
- Learning disabilities.
- Brain damage.
- Trouble walking.
- Seizures.
- Kidney failure.
- Shock.
- Death.
With prompt treatment, even people with severe meningitis can have good recovery.
Prevention
Common bacteria or viruses that can cause meningitis can spread through coughing, sneezing, kissing, or sharing eating utensils, a toothbrush or a cigarette.
These steps can help prevent meningitis:
- Wash your hands. Careful hand-washing helps prevent the spread of germs. Teach children to wash their hands often, especially before eating and after using the toilet, spending time in a crowded public place or petting animals. Show them how to thoroughly wash and rinse their hands.
- Practice good hygiene. Don't share drinks, foods, straws, eating utensils, lip balms or toothbrushes with anyone else. Teach children and teens to avoid sharing these items too.
- Stay healthy. Maintain your immune system by getting enough rest, exercising regularly, and eating a healthy diet with plenty of fresh fruits, vegetables and whole grains.
- Cover your mouth. When you need to cough or sneeze, be sure to cover your mouth and nose.
- If you're pregnant, take care with food. Reduce your risk of a listeria infection by cooking meat, including hot dogs and deli meat, to 165 degrees Fahrenheit (74 degrees Celsius). Avoid cheeses made from unpasteurized milk. Choose cheeses that are clearly labeled as being made with pasteurized milk.
Vaccinations
Some forms of bacterial meningitis are preventable with the following vaccinations:
- Haemophilus influenzae type b vaccine (Hib). The World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) recommend this vaccine for children starting at about 2 months of age. The vaccine also is recommended for some adults, including those who have sickle cell disease or AIDS and those who don't have a spleen.
- Pneumococcal conjugate vaccine (PCV15 or PCV20). These vaccines are part of the CDC recommended routine vaccination schedule for children younger than 2 years. They also are part of the recommended vaccine schedule for children age 2 through 18 who are at high risk of pneumococcal disease.
- Pneumococcal polysaccharide vaccine (PPSV23). Older children and adults who need protection from pneumococcal bacteria may receive this vaccine. The CDC recommends the PPSV23 vaccine for all adults older than 65; for younger adults and children age 2 and older who have weak immune systems or chronic illnesses such as heart disease, diabetes or sickle cell anemia; and for anyone who doesn't have a spleen.
-
Meningococcal conjugate vaccine (MenACWY). The CDC recommends that a single dose be given to children ages 11 to 12, with a booster shot given at age 16. If the vaccine is first given between ages 13 and 15, the booster is recommended between ages 16 and 18. If the first shot is given at age 16 or older, no booster is necessary.
This vaccine also can be given to children between the ages of 2 months and 10 years who are at high risk of bacterial meningitis or who have been exposed to someone with the disease. It's also used to vaccinate healthy but previously unvaccinated people who have been exposed in outbreaks.
- Serogroup B meningococcal vaccine (MenB). The CDC recommends this vaccine for adults and children 10 years and older who are at increased risk of meningococcal disease. They include adults and children with sickle cell disease, who have a damaged spleen or who have had their spleen removed. They also include people with the rare immune disorder called complement component deficiency or who take certain medicines. This vaccine may be recommended if you're in a population that's having an outbreak of serogroup B meningococcal disease.
Diagnosis
A health care provider can diagnose meningitis based on a medical history, a physical exam and certain tests. During the exam, your provider may check for signs of infection around the head, ears, throat and skin along the spine.
Common tests to diagnose meningitis include:
- Blood cultures. A blood sample is placed in a special dish to see if it grows microorganisms such as bacteria. This is called a blood culture. A sample also may be placed on a slide and stained. Then it will be studied under a microscope to see whether bacteria are present.
- Imaging. Computerized tomography (CT) or magnetic resonance imaging (MRI) scans of the head may show swelling or inflammation. X-rays or CT scans of the chest or sinuses may show an infection that may be associated with meningitis.
-
Spinal tap. A definitive diagnosis of meningitis requires a spinal tap to collect cerebrospinal fluid. In people with meningitis, the fluid often shows a low sugar level along with an increased white blood cell count and increased protein.
Analyzing the fluid also may help identify which bacterium caused the meningitis. If viral meningitis is suspected, you may need a DNA-based test known as a polymerase chain reaction amplification. Or you may be given a test to check for antibodies against certain viruses to determine the specific cause and proper treatment.
Treatment
The treatment depends on the type of meningitis you or your child has.
Bacterial meningitis
Acute bacterial meningitis must be treated right away with intravenous antibiotics and sometimes corticosteroids. This helps to ensure recovery and reduce the risk of complications, such as brain swelling and seizures.
The antibiotic or combination of antibiotics depends on the type of bacteria causing the infection. Your health care provider may recommend a broad-spectrum antibiotic until the exact cause of the meningitis is known.
Your provider may drain any infected sinuses or mastoids — the bones behind the outer ear that connect to the middle ear.
Viral meningitis
Antibiotics can't cure viral meningitis, and most cases improve on their own in several weeks. Treatment of mild cases of viral meningitis usually includes:
- Bed rest.
- Plenty of fluids.
- Pain medicine to help reduce fever and relieve body aches.
Your health care provider may prescribe corticosteroids to reduce swelling in the brain and a medicine to control seizures. If a herpes virus caused your meningitis, an antiviral medicine is available.
Other types of meningitis
If the cause of your meningitis is unknown, you may start antiviral and antibiotic treatment while the cause is determined.
Treatment for chronic meningitis is based on the underlying cause. Antifungal medicines treat fungal meningitis. A combination of specific antibiotics can treat tuberculous meningitis. However, these medicines can have serious side effects, so treatment may be deferred until a laboratory can confirm that the cause is fungal.
Noninfectious meningitis due to allergic reaction or autoimmune disease may be treated with corticosteroids. In some cases, no treatment may be required because the condition can resolve on its own. Cancer-related meningitis requires therapy for the specific cancer.
Preparing for an appointment
Meningitis can lead to death, depending on the cause. If you've been exposed to bacterial meningitis and you develop symptoms, go to an emergency room and tell the health care providers that you may have meningitis.
If you're not sure what you have and you call your provider for an appointment, here's how to prepare for your visit.
What you can do
- Be aware of any pre- or post-appointment restrictions. Ask if there's anything you need to do in advance, such as restrict your diet. Also ask if you may need to stay at your health care provider's office for observation following your tests.
- Write down symptoms you're having, including changes in your mood, thinking or behavior. Note when you developed each symptom and whether you had cold- or flu-like symptoms.
- Write down key personal information, including any recent moves, vacations or interactions with animals. If you're a college student, your provider likely will ask questions about any similar signs or symptoms in your roommates and dorm mates. Your provider also will want to know your vaccination history.
- Make a list of all medicines, vitamins or supplements you're taking.
- Take a family member or friend along. Meningitis can be a medical emergency. Take someone who can help remember all the information you may receive and who can stay with you if needed.
- Write down questions to ask your health care provider.
For meningitis, some basic questions to ask your health care provider include:
- What kinds of tests do I need?
- What treatment do you recommend?
- Am I at risk of long-term complications?
- If my condition is not treatable with antibiotics, what can I do to help my body recover?
- Am I contagious? Do I need to be isolated?
- What is the risk to my family? Should they take preventive medicine?
- Is there a generic alternative to the prescription medicine you're recommending?
- Do you have any printed information I can have? What websites do you recommend?
What to expect from your doctor
Your health care provider is likely to ask you a number of questions, such as:
- When did you begin experiencing symptoms?
- How severe are your symptoms? Do they seem to be getting worse?
- Does anything seem to improve your symptoms?
- Have you been exposed to anyone with meningitis?
- Does anyone in your household have similar symptoms?
- What is your vaccination history?
- Do you take any immunosuppressant medicines?
- Do you have other health problems, including allergies to any medicines?
What you can do in the meantime
When you call your health care provider's office for an appointment, describe the type and severity of your symptoms. If your provider says you don't need to come in immediately, rest as much as possible while you're waiting for your appointment.
Drink plenty of fluids and take acetaminophen (Tylenol, others) to reduce your fever and body aches. Also avoid any medicines that may make you less alert. Don't go to work or school.
© 1998-2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


