Overview
Postherpetic neuralgia (post-hur-PET-ik noo-RAL-juh) is the most common complication of shingles. It causes a burning pain in nerves and skin. The pain lasts long after the rash and blisters of shingles go away.
The risk of postherpetic neuralgia rises with age. It mainly affects people older than 60. There's no cure, but treatments can ease symptoms. For most people, postherpetic neuralgia gets better over time.
Symptoms
In general, the symptoms of postherpetic neuralgia are limited to the area of skin where the shingles outbreak first happened. That's commonly in a band around the trunk of the body, most often on one side.
The symptoms might include:
- Pain that lasts three months or longer after the shingles rash has healed. The pain may feel burning, sharp and jabbing. Or it may feel deep and aching.
- Not being able to stand light touch. People with postherpetic neuralgia often can't bear even the touch of clothing on the affected skin.
- Itching or loss of feeling. Less often, postherpetic neuralgia can cause an itchy feeling or numbness.
When to see a doctor
See a health care provider at the first sign of shingles. Often the pain starts before you notice a rash. The risk of postherpetic neuralgia becomes lower if you start taking virus-fighting medicines called antivirals within 72 hours of getting the shingles rash.
Causes
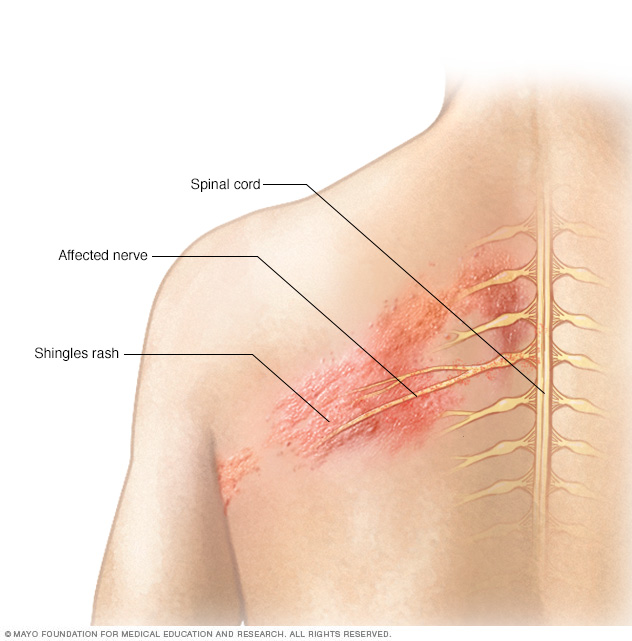
The chickenpox virus causes shingles. Once you've had chickenpox, the virus stays in your body for the rest of your life. The virus can become active again and cause shingles. This risk goes up with age. The risk also rises if something turns down the body's immune system, such as chemotherapy medicines to treat cancer.
Postherpetic neuralgia happens if nerve fibers get damaged during an outbreak of shingles. Damaged fibers can't send messages from the skin to the brain as they usually do. Instead, the messages become confused and heightened. This causes pain that can last months or even years.
Risk factors
With shingles, things that can raise the risk of postherpetic neuralgia are:
- Age. You're older than 60.
- How bad the case of shingles was. You had a severe rash and pain that kept you from doing daily activities.
- Other illness. You have a long-term disease, such as diabetes.
- Where shingles appeared. You had shingles on your face or torso.
- A delay in shingles treatment. You didn't start taking antiviral medicine within 72 hours of your rash appearing.
- No shingles vaccine. You had not been vaccinated for shingles.
Complications
People with postherpetic neuralgia can develop other problems that are common with long-term pain. It depends on how long the postherpetic neuralgia lasts and how painful it is. These other problems can include:
- Depression.
- Trouble sleeping.
- Tiredness
- Not feeling as hungry as usual.
Prevention
Shingles vaccines can help prevent shingles and postherpetic neuralgia. Ask your health care provider when you should get a vaccine.
In the United States, the Centers for Disease Control and Prevention (CDC) suggests that adults 50 and older get a shingles vaccine called Shingrix. The agency also suggests Shingrix for adults 19 and older who have weaker immune systems because of diseases or treatments. Shingrix is suggested even if you've already had shingles or the older vaccine, Zostavax. Shingrix is given in two doses, 2 to 6 months apart.
With two doses, Shingrix is more than 90% effective in preventing shingles and postherpetic neuralgia. Other shingles vaccines are offered outside of the United States. Talk to your provider for more information on how well they prevent shingles and postherpetic neuralgia.
Diagnosis
Your health care provider will check your skin. They might touch the skin in different places to find the borders of the affected area.
In most cases, no tests are needed.
Treatment
No single treatment relieves postherpetic neuralgia for everyone. It often takes a mix of treatments to ease the pain.
Lidocaine skin patches
These are small, bandage-like patches. They contain the pain-relieving medicine lidocaine. These patches can be cut to fit only the affected area. You put the patches on painful skin to get short-term relief. Your health care provider may prescribe them for you. Or you can buy the patches off the shelf at a slightly lower dose. Store them in a place that's away from children.
Capsaicin skin patch
Capsaicin comes from the seeds of hot chili peppers. A high amount of capsaicin is available as a skin patch to ease pain called Qutenza. You need to get it from your health care provider. A trained health care professional places the patch on your skin after using a medicine to numb the affected area.
The process takes at least two hours. That's because health care professionals need to watch for any side effects after the patch goes on. The patch lowers some people's pain for up to three months. If it works, you can get a new patch every three months.
Anticonvulsants
Some medicines for seizures also can ease the pain of postherpetic neuralgia. They include gabapentin (Neurontin, Gralise, others) and pregabalin (Lyrica). These medicines calm injured nerves. Side effects include:
- Feeling sleepy.
- Trouble thinking clearly.
- Not feeling steady.
- Swelling in the feet.
Antidepressants
Some depression medicines can do more than treat a mood disorder. They affect key brain chemicals that play a role in both depression and how the body interprets pain. They can help for pain even when you do not have depression. These medicines include:
- Nortriptyline (Pamelor).
- Amitriptyline.
- Duloxetine (Cymbalta).
- Venlafaxine (Effexor XR).
Health care providers often prescribe antidepressants for postherpetic neuralgia in smaller doses than they do for depression alone.
Common side effects of these medications include:
- Feeling sleepy.
- Getting a dry mouth.
- Feeling faint.
- Gaining weight.
Opioid painkillers
Opioids are very strong pain medicines that a health care provider can prescribe. Some people with postherpetic neuralgia might need medicines that contain tramadol (Conzip, Qdolo, others), oxycodone (Percocet, Oxycet, others) or morphine.
Opioids can cause side effects such as:
- A mild dizzy feeling.
- Sleepiness.
- Confusion.
- Trouble making bowel movements.
In the United States, the CDC urges health care providers to use opioids only for cancer-related problems and a few other serious health issues. The agency wants providers to think twice before they prescribe these powerful medicines for health problems such as postherpetic neuralgia. That's because opioids raise the risk of addiction and death in some people.
An opioid may be prescribed for postherpetic neuralgia only if safer treatments haven't worked. Before you start taking an opioid, your provider should:
- Explain the medicine's benefits and risks.
- Set up treatment goals for pain relief.
- Make a plan to help you safely stop using the medicine if the risks become too big.
Take the lowest possible dose of an opioid. And get checkups as often as your health care provider suggests.
Driving while on opioids can be dangerous. And it's not safe to take an opioid along with alcohol or other medicines.
Steroid shots
Shots of steroids into the spine may help some people with postherpetic neuralgia.
Lifestyle and home remedies
An over-the-counter medicine called capsaicin cream may ease the pain of postherpetic neuralgia. It's made from the seeds of hot chili peppers. Capsaicin (Capzasin-P, Zostrix, others) can cause a burning feeling and may bother your skin. These side effects usually fade over time. But you should use only a small amount when you first try it to make sure you don't have bad side effects.
Try not to get capsaicin cream on parts of your body that don't have symptoms. Follow all the instructions that come with the cream. Wear gloves when you put it on, and wash your hands afterward.
Preparing for an appointment
You might start by seeing your family health care provider. They may refer you to a nerve specialist called a neurologist. Or they might suggest you see a doctor who specializes in treating long-term pain.
Here's information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance. For instance, you may need to stop eating for a certain amount of time before you take a medical test. Make a list of:
- Your symptoms, including any that don't seem related to the reason for your checkup. Be sure to note when the symptoms began.
- Key personal information, including major stresses, recent life changes and family medical history.
- All medicines, vitamins or other supplements you take, including doses.
- Questions to ask your health care provider.
Take a family member or friend along if you can. A relative or friend can help you remember the information you're given.
For postherpetic neuralgia, questions to ask your doctor include:
- How long might my symptoms last?
- What treatment do you suggest? And are there other choices?
- I have other health problems. How can I best manage them together?
- Is there anything I shouldn't do while I recover?
- Should I see a specialist?
- Are there brochures or other printed material I can have? What websites do you recommend?
Feel free to ask other questions too.
What to expect from your doctor
Your doctor is likely to ask you questions such as:
- Do your symptoms happen some or all the time?
- How bad are your symptoms?
- Have you had chickenpox? When?
- Have you had a shingles vaccine?
- What, if anything, seems to improve your symptoms?
- What, if anything, seems to make your symptoms worse?
© 1998-2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


