Overview
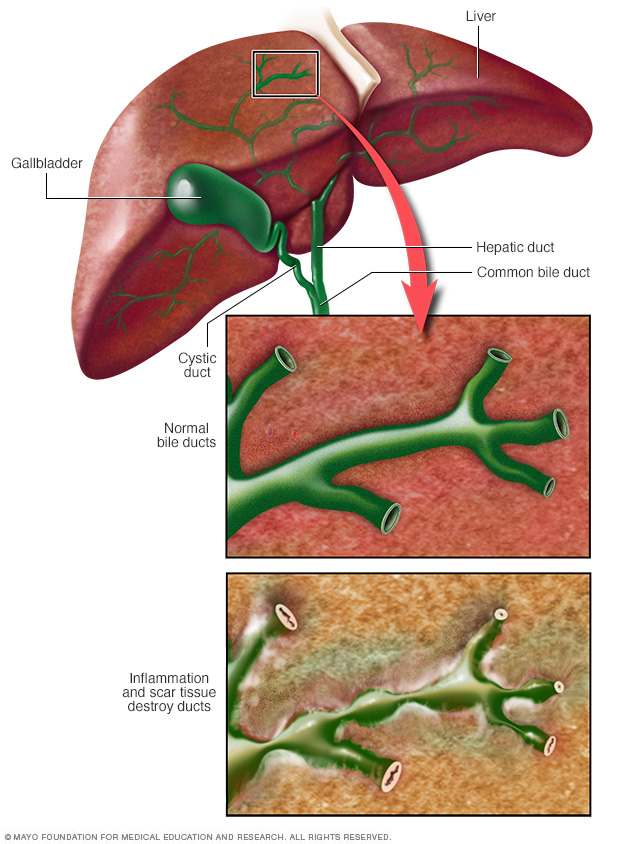
Primary sclerosing (skluh-ROHS-ing) cholangitis (koh-lan-JIE-tis) is a disease of the bile ducts. Bile ducts carry the digestive liquid bile from your liver to your small intestine. In primary sclerosing cholangitis, inflammation causes scars within the bile ducts. These scars make the ducts hard and narrow and gradually cause serious liver damage. A majority of people with primary sclerosing cholangitis also have inflammatory bowel disease, such as ulcerative colitis or Crohn's disease.
In most people with primary sclerosing cholangitis, the disease progresses slowly. It can eventually lead to liver failure, repeated infections, and tumors of the bile duct or liver. A liver transplant is the only known cure for advanced primary sclerosing cholangitis, but the disease may recur in the transplanted liver in a small number of patients.
Care for primary sclerosing cholangitis focuses on monitoring liver function, managing symptoms and, when possible, doing procedures that temporarily open blocked bile ducts.
Symptoms
Primary sclerosing cholangitis is often diagnosed before symptoms appear when a routine blood test or an X-ray taken for an unrelated condition shows liver abnormalities.
Early signs and symptoms often include:
- Fatigue
- Itching
- Yellow eyes and skin (jaundice)
- Abdominal pain
Many people diagnosed with primary sclerosing cholangitis before they have symptoms continue to feel generally well for several years. But there's no reliable way to predict how quickly or slowly the disease will progress for any individual.
Signs and symptoms that may appear as the disease progresses include:
- Fever
- Chills
- Night sweats
- Enlarged liver
- Enlarged spleen
- Weight loss
When to see a doctor
Make an appointment with your doctor if you have severe, unexplained itching on much of your body — itching that persists no matter how much you scratch. Also see your doctor if you feel extremely tired all the time, no matter what you do.
It's particularly important to bring unexplained fatigue and itching to your doctor's attention if you have ulcerative colitis or Crohn's disease, both of which are types of inflammatory bowel disease. A majority of people with primary sclerosing cholangitis also have one of these diseases.
Causes
It's not clear what causes primary sclerosing cholangitis. An immune system reaction to an infection or toxin may trigger the disease in people who are genetically predisposed to it.
A large proportion of people with primary sclerosing cholangitis also have inflammatory bowel disease, an umbrella term that includes ulcerative colitis and Crohn's disease.
Primary sclerosing cholangitis and inflammatory bowel disease don't always appear at the same time, though. In some cases, primary sclerosing cholangitis is present for years before inflammatory bowel disease occurs. If primary sclerosing cholangitis is diagnosed, it's important to look for inflammatory bowel disease because there is a greater risk of colon cancer.
Somewhat less often, people being treated for inflammatory bowel disease turn out to have primary sclerosing cholangitis as well. And rarely, people with primary sclerosing cholangitis develop inflammatory bowel disease only after having a liver transplant.
Risk factors
Factors that may increase the risk of primary sclerosing cholangitis include:
- Age. Primary sclerosing cholangitis can occur at any age, but it's most often diagnosed between the ages of 30 and 40.
- Sex. Primary sclerosing cholangitis occurs more often in men.
- Inflammatory bowel disease. A large proportion of people with primary sclerosing cholangitis also have inflammatory bowel disease.
- Geographical location. People with Northern European heritage have a higher risk of primary sclerosing cholangitis.
Complications
Complications of primary sclerosing cholangitis may include:
- Liver disease and failure. Chronic inflammation of the bile ducts throughout your liver can lead to tissue scarring (cirrhosis), liver cell death and, eventually, loss of liver function.
- Repeated infections. If scarring of the bile ducts slows or stops the flow of bile out of the liver, you may experience frequent infections in the bile ducts. The risk of infection is particularly high after you've had a surgical procedure to expand a badly scarred bile duct or remove a stone blocking a bile duct.
-
Portal hypertension. Your portal vein is the major route for blood flowing from your digestive system into your liver. Portal hypertension refers to high blood pressure in this vein.
Portal hypertension can cause fluid from the liver to leak into your abdominal cavity (ascites). It can also divert blood from the portal vein to other veins, causing these veins to become swollen (varices). Varices are weak veins and tend to bleed easily, which can be life-threatening.
- Thinning bones. People with primary sclerosing cholangitis may experience thinning bones (osteoporosis). Your doctor may recommend a bone density exam to test for osteoporosis every few years. Calcium and vitamin D supplements may be prescribed to help prevent bone loss.
- Bile duct cancer. If you have primary sclerosing cholangitis, you have an increased risk of developing cancer in the bile ducts or gallbladder.
- Colon cancer. People with primary sclerosing cholangitis associated with inflammatory bowel disease have an increased risk of colon cancer. If you've been diagnosed with primary sclerosing cholangitis, your doctor may recommend testing for inflammatory bowel disease, even if you have no signs or symptoms, since the risk of colon cancer is elevated if you have both diseases.
Diagnosis
Tests and procedures used to diagnose primary sclerosing cholangitis include:
- Liver function blood test. A blood test to check your liver function, including levels of your liver enzymes, can give your doctor clues about your diagnosis.
- MRI of your bile ducts. Magnetic resonance cholangiopancreatography (koh-lan-jee-o-pan-cree-uh-TOG-ruh-fee) uses magnetic resonance imaging (MRI) to make images of your liver and bile ducts and is the test of choice to diagnose primary sclerosing cholangitis.
-
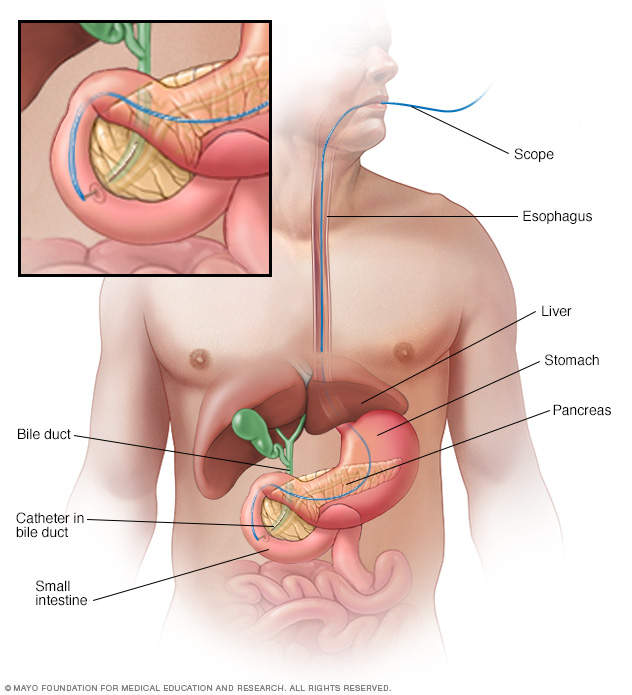
X-rays of your bile ducts. A type of bile duct X-ray called endoscopic retrograde cholangiopancreatography (ERCP) in addition to, or instead of, an MRI may be needed. But this test is rarely used for diagnosis because of the risk of complications.
To make your bile ducts visible on an X-ray, your doctor uses a flexible tube passed down your throat to inject dye into the area of your small intestine where your bile ducts empty.
An ERCP is the test of choice if signs and symptoms persist despite no abnormalities on an MRI. An ERCP is often the initial test if you're unable to have an MRI because of a metal implant in your body.
-
Liver biopsy. A liver biopsy is a procedure to remove a piece of liver tissue for laboratory testing. Your doctor inserts a needle through your skin and into your liver to extract a tissue sample.
A liver biopsy can help determine the extent of damage to your liver. The test is used only when the diagnosis of primary sclerosing cholangitis is still uncertain after less-invasive tests.
Treatment
Treatments for primary sclerosing cholangitis focus on managing complications and monitoring liver damage. Many medications have been studied in people with primary sclerosing cholangitis, but so far none have been found to slow or reverse the liver damage associated with this disease.
Treatment for itching
- Bile acid sequestrants. Medications that bind to bile acids — the substances thought to cause itching in liver disease — are the first line treatment for itching in primary sclerosing cholangitis.
- Antibiotics. If you have trouble tolerating a bile acid-binding drug or if it doesn't help, your doctor may prescribe rifampin (Rifadin, Rimactane, others), an antibacterial drug. Exactly how rifampin reduces itching is unknown, but it may block the brain's response to itch-inducing chemicals in your circulation.
-
Antihistamines. This type of medication may help reduce mild itching caused by primary sclerosing cholangitis. Whether these medications are effective for this condition is unknown.
Antihistamines may worsen the liver disease symptoms of dry eyes and dry mouth. On the other hand, antihistamines can help with sleep if itching keeps you awake.
- Opioid antagonists. Itching related to liver disease may also respond to opioid antagonist drugs, such as naltrexone. Like rifampin, these drugs seem to reduce the itch sensation by acting on your brain.
- Ursodeoxycholic acid (UDCA). Also known as ursodiol, UDCA is a naturally occurring bile acid that may help relieve itching symptoms caused by liver disease by increasing the absorbability of bile.
Treatment for infections
Bile that backs up in narrowed or blocked ducts causes frequent bacterial infections. To prevent and treat these infections, people with primary sclerosing cholangitis may take repeated courses of antibiotics or continue taking antibiotics for long periods.
Before any procedure that could cause an infection, such as an endoscopic procedure or abdominal surgery, you'll also need to take antibiotics.
Nutrition support
Primary sclerosing cholangitis makes it difficult for your body to absorb certain vitamins. Even though you may eat a healthy diet, you may find that you can't get all the nutrients you need.
Your doctor may recommend vitamin supplements that you take as tablets or that you receive as an infusion through a vein in your arm. If the disease weakens your bones, you may take calcium and vitamin D supplements as well.
Treatment for bile duct blockages
Blockages that occur in your bile ducts may be due to disease progression but can be a sign of cancer of the bile duct. Endoscopic retrograde cholangiopancreatography (ERCP) can help determine the cause, and bile duct blockage can be treated with:
- Balloon dilation. This procedure can open blockages in the larger bile ducts outside the liver. In balloon dilation, your doctor runs a slender tube with an inflatable balloon at its tip (balloon catheter) through an endoscope and into a blocked bile duct. Once the balloon catheter is in place, the balloon is inflated.
- Stent placement. In this procedure, your doctor uses an endoscope and attached instruments to place a small plastic tube called a stent in a blocked bile duct to hold the duct open.
Liver transplant
A liver transplant is the only treatment known to cure primary sclerosing cholangitis. During a liver transplant, surgeons remove your diseased liver and replace it with a healthy liver from a donor.
A liver transplant is reserved for people with liver failure or other severe complications of primary sclerosing cholangitis. Though uncommon, it's possible for primary sclerosing cholangitis to recur after a liver transplant.
Lifestyle and home remedies
If you've been diagnosed with primary sclerosing cholangitis, take steps to care for your liver, such as:
- Don't drink alcohol.
- Get vaccinated against hepatitis A and B.
- Use care with chemicals at home and at work.
- Maintain a healthy weight.
- Follow directions on all medications, both prescription and over-the-counter. Make sure your pharmacist and any doctor prescribing for you know that you have a liver disease.
- Talk to your doctor about any herbs or supplements you're taking since some can be harmful to your liver.
Alternative medicine
No alternative medicine treatments have been found to treat primary sclerosing cholangitis. But some complementary and alternative therapies may help you cope with the signs and symptoms of the disease. Talk to your doctor about your options.
Fatigue is common in people with primary sclerosing cholangitis. While doctors can treat some factors that may contribute to fatigue, your signs and symptoms may persist. You might find relief with complementary and alternative treatments that have shown some benefit for fatigue, such as:
- Regular exercise done more than two hours before you go to bed, which can help promote better sleep
- A well-balanced diet that includes fruit, vegetables, whole grains and protein
- Stress management techniques, such as meditation and relaxation exercises
Preparing for an appointment
Start by seeing your primary care doctor if you have signs or symptoms that worry you. If your doctor suspects you may have primary sclerosing cholangitis, you may be referred to a liver specialist (gastroenterologist or hepatologist).
Because appointments can be brief and because there's often a lot of ground to cover, it's a good idea to be well-prepared. Here's some information to help you get ready and what to expect from your doctor.
What you can do
- Be aware of any pre-appointment restrictions. When you make your appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medications, as well as any vitamins or supplements, that you're taking.
- Consider taking a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your doctor.
Your time with your doctor is limited. You may feel less rushed if you make a list of questions you want to ask at your appointment. Here are some possible questions about primary sclerosing cholangitis:
- Can you explain my test results to me?
- Will I need more tests?
- How far has my primary sclerosing cholangitis progressed?
- How severe is the damage to my liver?
- Can you estimate when I may need a liver transplant?
- What treatments can relieve my signs and symptoms?
- What are the potential side effects of each treatment?
- Should I be tested for inflammatory bowel disease?
- What signs and symptoms signal that my condition is worsening and I need to make another appointment?
- Are there any restrictions that I need to follow?
- Should I see a specialist?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask questions that come up during your appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may allow more time later to cover points you want to address. Your doctor may ask:
- When did you begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Do you have frequent bouts of diarrhea?
- Have you noticed blood in your stool?
© 1998-2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


