Overview
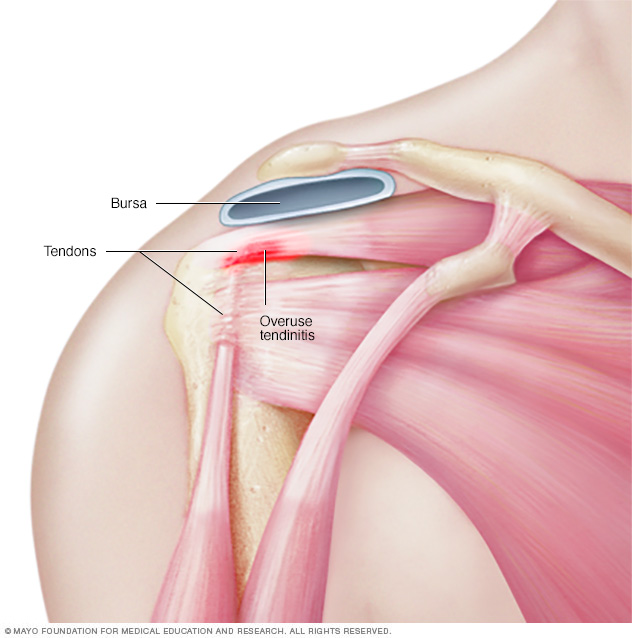
Tendinitis is inflammation of the thick fibrous cords that attach muscle to bone. These cords are called tendons. The condition causes pain and tenderness just outside a joint.
Tendinitis can occur in any tendon. But it's most common around shoulders, elbows, wrists, knees and heels.
Most tendinitis can be treated with rest, physical therapy and medicine to reduce pain. Long-lasting tendon inflammation can cause a tendon to tear. A torn tendon might need surgery.
Symptoms
Symptoms of tendinitis tend to occur where a tendon attaches to a bone. Symptoms often include:
- Pain, often described as a dull ache, especially when moving the hurt limb or joint
- Tenderness
- Mild swelling
When to see a doctor
Most cases of tendinitis respond to self care. See your health care provider if your symptoms don't lessen after a few days and if they get in the way of daily activities.
Causes
Tendinitis can be caused by a sudden injury. But repeating the same movement over time is a much more likely cause. Most people develop tendinitis because their jobs or hobbies involve motions that they repeat, over and over. This puts stress on tendons.
Moving correctly is especially important when having to repeat movements for sports or a job. Moving incorrectly can overload the tendon and lead to tendinitis.
Risk factors
Risk factors for developing tendinitis include age, having jobs that involve doing the same motion over and over, doing physical activities with poor form, and taking certain medicines.
Age
As people get older, their tendons become less flexible — which makes them easier to injure.
Work
Tendinitis is more common in people, such as gardeners and manual laborers, whose jobs involve:
- Repeated motions
- Awkward positions
- A lot of overhead reaching
- Vibration
- Forced movements
Activities
When doing physical activities, the following can increase the risk of tendinitis:
- Sudden increase in amount or difficulty of training
- Poor equipment, such as old shoes
- Hard surfaces, such as concrete or gym floors
- Too little recovery time after an injury or too little time to get used to the activity again after time off
- Poor posture or body movements
Medical condition and medications
Certain medical conditions, such as diabetes, can increase the risk of tendinitis. Medications that may increase risk include:
- Antibiotics known as fluoroquinolines
- Corticosteroids such as cortisone
- Aromatase inhibitors, used to lower breast cancer risk
Complications
Without treatment, tendinitis can increase the risk of a tendon breaking down or tearing. A completely torn tendon might need surgery.
Prevention
To reduce the chance of developing tendinitis, follow these suggestions:
- Ease up. Avoid activities that place too much stress on your tendons, especially for long periods. If you have pain during an exercise, stop and rest.
- Mix it up. If one exercise or activity causes you pain, try something else. Cross-training can help you mix high-impact exercise, such as running, with lower impact exercise, such as biking or swimming.
- Improve the way you move. If how you do an activity or exercise is flawed, you could be setting yourself up for problems with your tendons. Consider taking lessons or getting professional instructions when starting a new sport or using exercise equipment.
- Stretch. After exercise, move your joints through full range of motion. The best time to stretch is after exercise, when your muscles are warmed up.
- Move right in the workplace. Make sure your chair, keyboard and desktop are positioned correctly for your height, arm length and the tasks you do. This will help protect your joints and tendons from stress.
- Prepare your muscles to play. Strengthening muscles used in your activity or sport can help them bear the load better.
Diagnosis
Usually, a physical exam alone can diagnose tendinitis. X-rays or other imaging tests might be used to rule out other conditions that could be causing the symptoms.
Treatment
The goals of tendinitis treatment are to relieve pain and reduce irritation. Self-care, including rest, ice and pain relievers, might be all that's needed. But full recovery might take several months.
Medications
Medicines used to treat tendinitis include:
- Pain relievers. Aspirin, naproxen sodium (Aleve), ibuprofen (Advil, Motrin IB, others) or acetaminophen (Tylenol, others) may relieve tendinitis pain. Some of these drugs can cause stomach upset, or kidney or liver problems. Creams containing pain relievers can be applied to the skin. These products can help relieve pain and avoid the side effects of taking these drugs by mouth.
- Steroids. A steroid shot around a tendon might help ease the pain of tendinitis. These shots aren't for tendinitis lasting more than three months. Repeated steroid shots can weaken a tendon and increase the risk of the tendon tearing.
- Platelet-rich plasma. This treatment involves taking a sample of your own blood and spinning the blood to separate out the platelets and other healing factors. The solution is then injected into the area of chronic tendon irritation. Though research is still going on to find the best way to use platelet-rich plasma, it has shown promise in the treatment of many chronic tendon conditions.
Physical therapy
Physical therapy exercises can help strengthen the muscle and tendon. Eccentric strengthening, which emphasizes contraction of a muscle while it's lengthening, is an effective treatment for many chronic tendon conditions.
Surgical and other procedures
In situations where physical therapy hasn't resolved symptoms, your health care provider might suggest:
- Dry needling. This procedure, usually performed with ultrasound to guide it, involves making small holes in the tendon with a fine needle to stimulate factors involved in tendon healing.
- Surgery. Depending on the severity of your tendon injury, surgical repair may be needed, especially if the tendon has torn away from the bone.
Lifestyle and home remedies
To treat tendinitis at home, use rest, ice, compression and elevation. This treatment can help speed recovery and help prevent more problems.
- Rest. Avoid doing things that increase the pain or swelling. Don't try to work or play through the pain. Healing requires rest, but not complete bed rest. You can do other activities and exercises that don't stress the injured tendon. Swimming and water exercise may be good options.
- Ice. To decrease pain, muscle spasm and swelling, apply ice to the injured area for up to 20 minutes several times a day. Ice packs, ice massage or slush baths with ice and water all can help. For an ice massage, freeze a paper cup full of water so that you can hold the cup while applying the ice directly to the skin.
- Compression. Because swelling can cause loss of motion in an injured joint, wrap the area tightly until the swelling stops. Use wraps or elastic bandages.
- Elevation. If tendinitis affects your knee, raise the hurt leg above the level of your heart to reduce swelling.
Although rest is a key to treating tendinitis, not moving joints can cause them to become stiff. After a few days of resting the injured area, gently move it through its full range of motion to keep your joints flexible.
Preparing for an appointment
You might start by talking to your family health care provider. But you may be referred to a specialist in sports medicine or rheumatology, the treatment of conditions that affect the joints.
What you can do
You may want to write a list that includes:
- Details about your symptoms
- Other medical problems you've had
- Medical problems your parents, brothers and sisters have had
- All the medicines and vitamins you take, including doses
- Questions you want to ask the care provider
For tendinitis, some basic questions to ask include:
- What is the most likely cause of my symptoms?
- Are there other possible causes?
- What tests do I need?
- What treatment do you recommend?
- I have other medical problems. How best can I manage them together?
- Will I need to limit my activities?
- What self-care can I do at home?
What to expect from your doctor
Your provider is likely to ask you questions, such as:
- Where do you feel pain?
- When did your pain begin?
- Did it begin all at once or come on bit by bit?
- What kind of work do you do?
- What are your hobbies? What do you do for fun?
- Have you been instructed in proper ways to do your activity?
- Does your pain occur or worsen during certain activities, such as kneeling or climbing stairs?
- Have you recently had a fall or other kind of injury?
- What treatments have you tried at home?
- What did those treatments do?
- What, if anything, makes your symptoms better?
- What, if anything, makes your symptoms worse?
© 1998-2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


